Community Intervention Hiv Msm 2015 Art With Condom Use
- Research article
- Open up Access
- Published:
Condom use in combination with ART tin can reduce HIV incidence and bloodshed of PLWHA among MSM: a study from Beijing, Cathay
BMC Infectious Diseases volume 18, Article number:124 (2018) Cite this article
Abstract
Background
Safe use and antiretroviral therapy (Art) are effective means to prevent and control HIV transmission. We aimed to assess the effect of condom use in combination with antiretroviral therapy (Fine art) on HIV incidence and mortality amid men who had sex with men (MSM) in Beijing, Communist china.
Methods
We evaluated the effect of prophylactic apply, ART, and the combination of both among people living with HIV/AIDS (PLWHA) of MSM in the Chaoyang District of Beijing using the Asian Epidemic Model (AEM). Evaluation indicators included absolute gamble reduction (ARR) and the percent of relative risk reduction (RRR %).
Results
HIV incidence and prevalence declined essentially when condoms were used by MSM in Chaoyang from 2003 to 2013. The ARR of HIV incidence was from 0 to 0.91% and the RRR% was from 0 to 43.93%. The ARR of HIV prevalence was from 0 to 3.79% and the RRR% was from 0 to 31.53%. The HIV mortality charge per unit decreased substantially (ARR from 0 to i.75%, and RRR% from 0 to 40.03%) when Fine art was implemented. When prophylactic use combined with ART was implemented in MSM in 2003–2013, HIV incidence declined substantially (ARR from 0 to 0.99%, and RRR% from 0 to 46.11%). HIV prevalence was also reduced with an ARR from 0 to 3.v%, and an RRR% from 0 to 29.88%. The HIV mortality too declined essentially (ARR from − 0.01% to 1.02%, RRR% from − 1.44% to 39.98%).
Conclusions
Among MSM, a combination of rubber utilise and Fine art reduces both HIV incidence and bloodshed caused past HIV. Combining these methods results in a more effective prevention and control of HIV.
Background
High-risk behaviour intervention is ane of the most effective ways to prevent and command HIV transmission [ane]. Condom use is an effective method to preclude the sexual transmission of HIV, the effect of which has been clearly demonstrated in People's republic of china [2]. Antiretroviral therapy (Fine art) tin can effectively decrease the viral load in the claret and trunk fluids of people living with HIV/AIDS (PLWHA), thereby reducing HIV manual [3, 4] and mortality. Currently, Pre-Exposure Prophylaxis (PrEP) has been gradually implemented as a preventative mensurate in populations at loftier risk of HIV infection [5]. ART was starting time introduced in 2003 in Chaoyang Commune, Beijing. With the implementation of the national policy "Four Frees and One Care" and the aligning of the initial eligibility threshold for therapy, [half-dozen] Art coverage increased yearly, with larger numbers of PLWHA benefiting from ART. Fine art has been shown to prolong the survival of PLWHA and to improve the quality of life [7].
Chaoyang Commune, located in the northeast of Beijing, covers an expanse of 470.8 km2. Notably, Chaoyang is the largest urban district of Beijing with a population of 5,050,000, which is approximately i-fourth of the capital'south full population. The first example of HIV infection in Chaoyang was reported in 1990. By December 31, 2014, a total of 5481 PLWHA cases had been reported in Chaoyang, with male homosexual transmission bookkeeping for 71.2% of all cases [viii]. HIV-positive men who had sex with men (MSM) comprised the largest contingent of HIV infections. In 2003, Chaoyang District implemented the National AIDS Comprehensive Prevention and Command Sit-in Pilot Projection. The project focused on peer instruction, safe use among MSM, and ART among PLWHA. As the project progressed, the rates of condom use and Art coverage improved amongst MSM in the area.
We used the Asian Epidemic Model (AEM) [9] to evaluate rubber utilise, Fine art, and the combined event of both methods on PLWHA who were MSM. The AEM was primarily adult to estimate epidemics and to simulate the spread of HIV in Asian countries [9,10,11]. With this model, we used the concept of "a Cause-Deleted Life Table" in a fixed area [12] and a relatively stable population to estimate the consequence of the in a higher place methods on HIV incidence and HIV-related deaths of PLWHA.
Methods
Aim
We aimed to assess the effect of condom use in combination with antiretroviral therapy (Art) on HIV incidence and mortality from 2003 to 2013 amidst MSM in Beijing.
Study design
The Asian epidemic model
The model nosotros used to evaluate the effectiveness of interventions was AEM (version 4.0), which was developed past Dr. Tim Brown et al., with support from the United States Bureau for International Development (USAID). AEM is a full procedure model that is used to estimate and projection the spread of HIV and to appraise interventions in Asian areas [13]. The model calculates the numbers of new HIV infections in each subgroup based on dissimilar routes of transmission. Information technology can as well be used to calculate the number of current HIV infections and HIV-related deaths [14].
- (1)
Calculation of the number of new HIV infections.
The number of new HIV infections (new HIV cases in one year) was calculated based on sexual frequency, multiplying the probability of HIV infections per dangerous behaviour and corrections for co-infection with HIV transmission.
For example, the number of new sexual infections of clients by straight sex workers was calculated every bit previously described [10]:
$$ \mathrm{n}={\mathrm{p}}_{{\mathrm{f}}_{\mathrm{m}}}{\mathrm{X}}_1{\mathrm{Five}}_{one\mathrm{a}}(t)\left(1-{\mathrm{C}}_{1\mathrm{a}}(t)\right)\left(\frac{{\mathrm{Y}}_{3\mathrm{a}}}{{\mathrm{X}}_{3a}+{\mathrm{Y}}_{iii\mathrm{a}}}\right)\mathrm{ten}\left[{\mathrm{C}}_{\mathrm{std}\_\mathrm{m}}{\mathrm{F}}_{\mathrm{std}\mathrm{a}(t)}+\left(1-{\mathrm{F}}_{\mathrm{std}\mathrm{a}}(t)\right)\right]+\left[{\mathrm{C}}_{\mathrm{cc}}{\mathrm{F}}_{\mathrm{cc}}(t)+\left(1-{\mathrm{F}}_{\mathrm{cc}}(t)\right)\right] $$
101 was the number of uninfected clients, Five1a(t) was the frequency of contact with sex workers, C1a(t) was the level of condom use, and X3a and Y3a were the number of uninfected and infected direct sex workers. The additional components [Cstd_mFstda(t) + (1 − Fstda(t))] and [CccFcc(t) + (1 − Fcc(t))] at the end of the expression represented the adjustments to the transmission for STD enhancement of transmission and the influence of circumcision, respectively.
The number of new HIV infections in each subgroup by different routes of transmission was calculated in the same way.
- (two)
Calculation of the number of current HIV infections (people living with HIV/AIDS), AIDS patients, and HIV-related deaths.
After the number of new HIV infections was calculated in each subgroup for each twelvemonth, nosotros could determine the numbers of new AIDS- and HIV-related deaths based on the progression of an HIV infection developing into AIDS and resulting in death. We obtained the number of current HIV infections using the cumulative HIV infections minus the sum of new AIDS- and HIV-related deaths.
We obtained the number of new HIV infections, electric current HIV infections, and HIV-related deaths among MSM during 2003–2013 from the results of the full general population in Chaoyang District. Nosotros then changed the input on behavioural and Fine art parameters and ran the AEM programme again. Adjacent, nosotros adamant annual HIV infections and HIV-related deaths nether different levels of ART and rubber utilise. The difference between these two results was taken to represent the effect of behaviour and handling intervention [9].
Source of data [fifteen]
We divided the population into the post-obit iv subgroups according actual transmission route in Chaoyang: (i) female sexual practice workers (FSW) and clients through heterosexual behaviour; (ii) MSM including male sex workers (MSW) through homosexual behaviour; (three) IV drug users (IDU) past sharing syringes; and (4) the general population.
- 1.
Population size: Demographic data were derived from the Statistical Yearbooks (1990 to 2010) of the Chaoyang District of Beijing, China [sixteen, 17].
- 2.
Behavioural parameters: Data related to the trends in behavioural changes, including condom use (2003 to 2013) (Table ane), proportions of needle sharing among IDUs (1999 to 2012), and sexual behaviour among IDUs and sex workers (1999 to 2010), were primarily derived from scout surveillance programmes offered by the Beijing Chaoyang Commune Center for Disease Command and Prevention [8, 18,19,xx,21,22].
- 3.
HIV prevalence: Data on HIV prevalence was collected from the relevant population groups including FSW, IDU, and MSM at the sentinel surveillance points (2003 to 2013) in the Chaoyang District of Beijing [23,24,25,26] (as shown in Table 1).
- 4.
Fine art-related parameters: Fine art coverage information (2003–2013) was obtained from the Report of Beijing Chaoyang District Wellness Bureau, and other ART-related parameters were obtained from the Beijing Chaoyang District AIDS Comprehensive Prevention Information System in Cathay (2003 to 2013) and other published references (Table 1) [27, 28].
- v.
Epidemiological parameters: Probabilities of HIV transmission via different routes, including vaginal intercourse transmission from males to females, vaginal intercourse manual from females to males, transmission from anally insertive partners to receptive partners, transmission from anally receptive partners to insertive partners, and shared needles for intravenous drug injections, were from published references [29,30,31,32].
Setting of the report
Enquiry hypothesis
We used AEM to estimate the numbers of new HIV infections, current HIV infections, and HIV-related deaths amidst MSM in Chaoyang. The estimated results were identified considering of the combined intervention of AIDS in Chaoyang in this study.
We divided MSM into unlike scenarios based on the intervention measures: with comprehensive intervention, without condom use, without Fine art, and without a combination of both safe utilize and ART. Nosotros analysed the differences between new HIV infections, electric current HIV infections, and HIV-related deaths.
Determining the consequence of comprehensive interventions: we assumed that the estimated numbers of new HIV infections, current HIV infections, and HIV-related deaths amidst MSM in 2003–2013 based on the AEM were the effect of comprehensive interventions.
Determining the consequence of interventions other than condom utilize: nosotros assumed that the rate of condom apply per twelvemonth remained at the level of 2003 (the rate of condom use per year between MSM and MSM was 42.00%; betwixt MSM and MSW, the charge per unit was 55.00%). Holding other factors unchanged, we calculated the numbers of new HIV infections, current HIV infections, and HIV-related deaths among MSM from 2003 to 2013, which nosotros considered to be the outcome of other interventions autonomously from condom utilise.
Determining the effect of interventions other than ART: we assumed that ART coverage and the CD4 threshold for treatment eligibility amongst PLWHA of MSM remained the same as the 2003 level (ART coverage was 5.06%; CD4 cell count ≤200 cells/μl). Belongings other factors unchanged, we calculated the numbers of new HIV infections, current infections, and HIV-related deaths amidst MSM in 2003–2013, which we considered to be the effect of other interventions apart from ART.
Determining the event of interventions other than combined condom use and Art: we causeless that Art coverage, the CD4 threshold for treatment eligibility amid PLWHA of MSM, and the rate of condom utilise remained at the same level as 2003 (Fine art coverage was 5.06%; CD4 prison cell count ≤200 cells/μl; the rate of condom use between MSM and MSM was 42.00%; the rate of condom use between MSM and MSW was 55.00%). With other factors held unchanged, we calculated the numbers of new HIV infections, electric current HIV infections and HIV-related deaths among MSM in 2003–2013, which we considered to be the effect of other interventions autonomously from a combination of condom use and Art.
Assessing index
In this study, we used absolute take chances reduction (ARR) and relative risk reduction percentage (RRR%) to represent the consequence of interventions. ARR is the absolute divergence between rates of event incidence without and with an intervention. A larger ARR indicates a more effective intervention. The RRR% is a decision of the decrease in the relative risk of an adverse event (eastward.g., HIV infection) compared to the risk of an agin event pre-intervention. Thus, the RRR% indicates a reduction in the degree of relative risk before and later on an intervention.
The "events" in the post-obit formula referred to new HIV infections, current HIV infections and HIV-related death.
Effect of safe use among MSM:
ARR = Event rates without condom apply minus event rates with comprehensive interventions.
$$ RRR={\frac{\mathrm{Event}\ \mathrm{rates}\ \mathrm{with}\mathrm{out}\ \mathrm{condom}\ \mathrm{utilize}\hbox{-} \mathrm{effect}\ \mathrm{rates}\ \mathrm{with}\ \mathrm{comprehensive}\ \mathrm{interventions}}{Due east\mathrm{vent}\ \mathrm{rates}\ \mathrm{with}\mathrm{out}\ \mathrm{safety}\ \mathrm{use}}}^{\ast }100\% $$
Result of ART among PLWHA of MSM:
ARR = Effect rates without ART minus event rates with comprehensive interventions.
$$ RRR={\frac{\ \mathrm{Event}\ \mathrm{rates}\ \mathrm{with}\mathrm{out}\ \mathrm{ART}\hbox{-} \mathrm{event}\ \mathrm{rates}\ \mathrm{with}\ \mathrm{comprehensive}\ \mathrm{interventions}}{\mathrm{Consequence}\ \mathrm{rates}\ \mathrm{with}\mathrm{out}\ \mathrm{ART}}}^{\ast }100\% $$
Consequence of condoms in combination with Art amid MSM:
ARR = Event rates without condoms in combination with Art minus event rates with comprehensive interventions.
$$ RRR={\frac{\mathrm{Issue}\ \mathrm{rates}\ \mathrm{with}\mathrm{out}\kern0.5em \mathrm{condom}\ \mathrm{in}\ \mathrm{combination}\ \mathrm{with}\ \mathrm{ART}\hbox{-} \mathrm{upshot}\ \mathrm{rates}\ \mathrm{with}\ \mathrm{comprehensive}\ \mathrm{in}\mathrm{terventions}}{\mathrm{Event}\ \mathrm{rates}\ \mathrm{with}\mathrm{out}\ \mathrm{safety}\ \mathrm{in}\ \mathrm{combination}\ \mathrm{with}\ \mathrm{Fine art}}}^{\ast }100\% $$
Modelling process
In this study, we used AEM to appraise the affect of condom use in combination with Art on HIV incidence and mortality among MSM in Beijing.
First, we filled in many fundamental inputs, including population size, behavioural parameters, HIV prevalence, Art-related parameters, and epidemiological parameters, which were shown in the "source of data." Later on running the AEM, nosotros gained much data nearly the number of new HIV infections, current HIV infections, and HIV-related deaths among MSM during 2003–2013 in the Chaoyang District of Beijing. This was a issue of the status of the HIV epidemic with comprehensive interventions amid MSM.
Next, we reset the inputs on the charge per unit of condom utilise from 2003 to 2013 amid MSM (remained at the level of 2003) in AEM and maintained the other inputs unchanged to allow for the analysis of the downstream touch on of other interventions apart from condom use.
Then, we fabricated an adjustment to the inputs on the Fine art coverage and the handling eligibility from 2003 to 2013 (the same as the 2003 level) and held other inputs unchanged. We ran the AEM once once again and obtained the effect of other interventions apart from ART.
Lastly, we readjusted the inputs both on the charge per unit of condom apply amidst MSM and on the Art coverage and the handling eligibility from 2003 to 2013; the other factors remained unchanged. We obtained the effect of the other interventions apart from a combination of condom use and Fine art.
Results
Through model fitting, nosotros institute that when condoms were used, HIV incidence decreased essentially among MSM between 2003 and 2013 in Chaoyang, with an ARR from 0 to 0.91%, and an RRR% from 0 to 43.93%. HIV prevalence also declined with an ARR of 0~ 3.79% and an RRR% of 0~ 31.53% between 2003 and 2013. HIV mortality showed a rising trend with ARR from -0.61% to 0% and RRR% from − one.44% to 35.71% (Table 2, Figs. ane and ii).
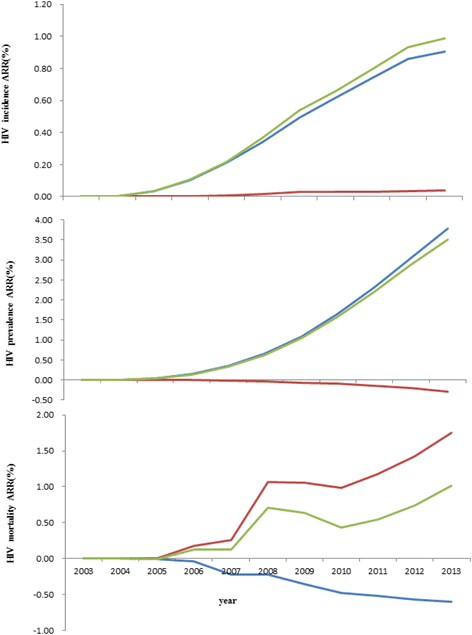
Impact of safety use, ART and combination of both on ARR of HIV infections among MSM and HIV mortality among PLWHA of MSM in 2003–2013.  Safe utilise,
Safe utilise,  Art,
Art,  ART combined with condom use
ART combined with condom use
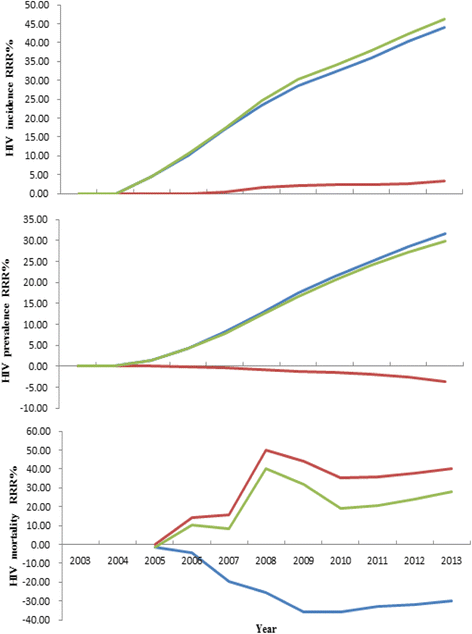
Impact of safe use, ART and combination of both on RRR% of HIV infections among MSM and HIV mortality among PLWHA of MSM in 2003–2013.  Condom use,
Condom use,  ART,
ART,  ART combined with condom use
ART combined with condom use
HIV incidence declined slightly with Fine art implementation amidst PLWHA of MSM in 2003–2013 in Chaoyang Commune. The ARR was from 0 to 0.04%, with an RRR% from 0 to three.23%. HIV prevalence increased slightly, with ARR from − 0.29% to 0 and RRR% from 0 to 3.69%. HIV bloodshed decreased substantially. The ARR was from 0 to i.75% and the RRR% was from 0 to forty.03% (as shown in Table 3, Figs. 1 and ii).
HIV incidence declined substantially with a combination of Art and condom use among PLWHA of MSM in 2003–2013. The ARR was from 0 to 0.99% and the RRR% was from 0 to 46.xi%. HIV incidence decreased slightly with ARR from 0 to 3.5% and RRR% from 0 to 29.88%. HIV mortality decreased substantially with ARR from − 0.01% to one.02% and RRR% from-ane.44% to 39.98% (as shown in Table four, Figs. 1 and ii).
Discussion
MSM maintain a relatively private status in China. Information technology is challenging to diagnose HIV infections and later deport out interventions aimed at reducing high-risk behaviour amid MSM and implementing ART among PLWHA. We accept used AEM to evaluate HIV preventive measures undertaken among MSM in 2003–2013 in Chaoyang, the district with the largest population in Beijing, based on customs population statistics. Modelling data was obtained from community demography data of Chaoyang, routine monitoring data of HIV infection condition among MSM, special investigations, data from voluntary consultation tests, and published references. This study should provide useful reference information for adjustments of future interventions to prevent the spread of HIV among MSM.
The MSM population has been recognized as the main source of new HIV infections in Chaoyang since 2001. Reducing HIV transmission among MSM can effectively control the progression of the HIV/AIDS epidemic in the commune [32]. Rubber use and ART were implemented among the MSM population from 2003 to 2013 in the Chaoyang Commune of Beijing. Compared with 2012, HIV incidence among MSM declined in 2013 and reached the target of the National AIDS Comprehensive Prevention and Control Demonstration Expanse (HIV incidence rates were reduced past xx%–25%) [33]. As shown in Table two to Tabular array four, we found that the decline of HIV incidence was estimated to take occurred without safety use and/or Art. One explanation could be that the exposure opportunities of the MSM population decreased due to increasing knowledge and the level of AIDS prevention in high-risk groups, including IDU, FSWs and multiple partners, in addition to the MSM population, along with the improvement of the AIDS prevention level in the whole customs.
The rates of prophylactic use between MSM and MSM during sex increased from 42.00% to 56.00% in 2003–2013. The rates of condom use likewise increased from 55.00% to 66.70% between MSM and MSW in 2003–2013. Our electric current data demonstrate that a unproblematic increase in condom use among MSM resulted in a significant decrease in the relative risk of new HIV infections with an RRR% of 0 to 43.93%. Condom use also resulted in a subtract in the relative take a chance of electric current HIV infections from 0 to 31.53%. This finding is consistent with results from previous studies [34]. Withal, this study also establish that the accented risk of HIV-related expiry among PLWHA who are MSM increased slightly from 0 to 0.61% in 2003–2013 due to an increase in condom use. The relative risk of HIV-related death besides increased slightly from 1.44% to 35.71%. Possible reasons for the increase in bloodshed were that the increase in condom use had no direct effect on HIV-related death among PLWHA with a large impact on reducing new HIV infections. It acquired the number of new HIV infections to decrease, resulting in an almanac reduction in the number of electric current HIV infections, thus leading to the increase in HIV mortality.
Fine art was offset implemented in 2003 in Chaoyang. ART coverage increased from an initial 5.06% to 29.72% in 2013. ART coverage benefited from increased Voluntary Counselling and Testing (VCT) and regular follow-up visits to patients to promote Art treatment amidst those who qualified for the treatment standard. Our results suggest that HIV incidence amidst MSM was reduced with the implementation of ART in 2003–2013, which agrees with previous studies [35, 36]. In our study, we found that ART had limited effects in reducing new HIV infections, and the ARR pct was from 0 to 0.04% and the RRR percentage was from 0 to iii.23%. It is possible that the effect of ART had non even so been given total attending because the coverage rate of Fine art was low in 2003–2013 in this area. Additionally, HIV mortality among MSM was dramatically decreased (RRR% from 0 to xl.03%), while both the HIV prevalence and the number of infection sources increased. We constitute that compared to condom utilize, the result of Fine art on reducing new HIV infections was lower, while the effect of ART in reducing HIV bloodshed was greater, and HIV mortality clearly decreased afterward Fine art implementation.
Our study also found that the effect of rubber use in combination with ART on reducing HIV incidence and HIV mortality was greater than the cumulative outcome of either Fine art lone or rubber apply alone in 2003–2013. Based on the above results, safety use in combination with ART is more constructive in preventing the spread of HIV among MSM in Chaoyang. Similar results were reported in the written report [37] by Ramadanovic B, which suggested that expanding ART coverage combined with interventions targeting loftier-take chances behaviours amplify the preventive bear upon.
We acknowledge that this study has several limitations. The AEM is a semi-empirical model, then its effects on the estimation of HIV/AIDS epidemics and the assessment of interventions are restricted by the limitations of the design itself and the experience of the experts involved. In this report, HIV mortality was calculated by HIV deaths/PLWHA/year in AEM, and a more useful measure of the event of the interventions on HIV mortality would be HIV deaths/100,000 population/year. In addition, this study does not take the influence of heterosexual behaviour of bisexual people among MSM into consideration. The number of heterosexual partners such as FSW and changes in their loftier-hazard behaviour may impact HIV infections amid MSM. Moreover, nosotros did not consider drug resistance and ART failure, which may theoretically influence the efficacy of Fine art.
Conclusions
In decision, interventions aimed at preventing HIV spread among MSM were effective in the Chaoyang District of Beijing in 2003–2013. Condom use can reduce the absolute and relative risk of HIV incidence and HIV prevalence. ART decreased the absolute risk and relative chance percentage of HIV mortality amongst PLWHA of MSM. Amidst MSM, condom use in combination with ART not simply reduces HIV incidence just also reduces HIV mortality, and it is more constructive in the prevention and control of the spread of HIV.
Abbreviations
- AEM:
-
Asian Epidemic Model
- ARR:
-
Absolute hazard reduction
- Fine art:
-
Antiretroviral therapy
- FSWs:
-
Female sex activity workers
- IDU:
-
4 drug user
- MSM:
-
Men who had sex with men
- MSW:
-
Male sex worker
- PLWHA:
-
People living with HIV/AIDS
- RRR:
-
Relative risk reduction
- USAID:
-
U.s.a. Agency for International Development
References
-
Baggaley RF, Garnett GP, Ferguson NM. Modelling the touch of antiretroviral utilise in resource-poor settings. PLoS Med. 2006;3:e124.
-
Zunyou W. Achievement of HIV AIDS plan in the past years and challenges in China. Chinese Journal Of Epidemiology. 2015;36
-
Smith JA, Sharma M, Levin C, Baeten JM, van Rooyen H, Celum C, et al. Cost-effectiveness of customs-based strategies to strengthen the continuum of HIV care in rural South Africa: a health economic modelling analysis. Lancet Hiv. 2015;ii:e159–68.
-
Rodger AJ, Cambiano Five, Bruun T, Vernazza P, Collins S, van Lunzen J, et al. Sexual activity without condoms and risk of HIV manual in Serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA. 2016;316:171–81.
-
Harries Advertizing, Lawn SD, Suthar AB, Granich R. Benefits of combined preventive therapy with co-trimoxazole and isoniazid in adults living with HIV: time to consider a fixed-dose, single tablet coformulation. Lancet Infect Dis. 2015;15:1492–vi.
-
Zhang Fujie WYYL. Antiretroviral Therapy for HIV/AIDS and Current State of affairs of Mainland china Gratuitous ARV Programme. Science & Engineering science Review 2005,23:24–28.
-
Zhang F, Dou Z, Ma Y, Zhang Y, Zhao Y, Zhao D, et al. Consequence of earlier initiation of antiretroviral handling and increased treatment coverage on HIV-related mortality in Mainland china: a national observational cohort report. Lancet Infect Dis. 2011;eleven:516–24.
-
Vocal Liang HYJS. Study on HIV and syphilis infections and related risk behaviors among male sex workers in Beijing, Communist china. Chinese J Epidemiol. 2012;33:640–2.
-
Dark-brown T, Peerapatanapokin W. The Asian epidemic model: a process model for exploring HIV policy and programme alternatives in Asia. Sex Transm Infect. 2004;80(Suppl 1):i19–24.
-
Mishra RM, Dube M, Sahu D, Saggurti N, Pandey A. Changing epidemiology of HIV in Mumbai: an application of the Asian epidemic model. Glob J Wellness Sci. 2012;4:100–12.
-
Ma Due north, Zheng M, Liu G, et al. Affect of safety utilise and standardized sexually transmitted disease treatment on HIV prevention amid men who accept sex with men in Hunan province: using the Asian epidemic model[J]. AIDS Res Hum Retrovir. 2012;28(10):1273–nine.
-
Katzmarzyk PT, Lee IM. Sedentary behaviour and life expectancy in the The states: a cause-deleted life tabular array analysis. BMJ Open up. 2012;2
-
Cohen J. The Asian epidemic model's provocative curves. Science. 2004;304:1934.
-
Yu Da LMMZ. A process model for exploring the effectiveness of HIV prevention and control policies and programs -- an introduction to the Asian epidemic model (AEM). Chin J AIDS STD. 2008;96-97(65):xiv.
-
Tao LL, Liu M, Li SM, Liu J, Jiang SL, Wang LJ, et al. Touch of antiretroviral therapy on the spread of human immunodeficiency virus in Chaoyang Commune, Beijing, China: using the Asian epidemic model. Chin Med J. 2017;130:32–8.
-
Beijing City TCDB. The fifth census of Beijing Chaoyang Commune role, Beijing Chaoyang District 2000 census information. In. 2002;
-
Beijing City TCDB. The 6th census of Beijing Chaoyang District office, Beijing Chaoyang District 2010 census data. In. 2012;
-
Pan Suiming WWAL. Sexual behavior and sexual relationship in gimmicky Chinese. Beijing: Social Sciences Bookish Press; 2004.
-
Li Dongliang DHLF. An epidemiological analysis of sexual transmitted diseases among 1512 cases of female person sex workers. China Journal of Leprosy and Pare Diseases. 2006;22:576–7.
-
THE THAI WORKING Grouping PROJECTIONS. The Asian Epidemic Model (AEM) Projections for HIV/AIDS in Thailand: 2005-2025. In; 2005.
-
Dongliang L, Zheng Z, Fengji L. Surveillance analysis of prevalence of sexually transmitted affliction in Beijing Chaoyang district from 1993 to 2003. Chinese Journal of AIDS & STD 2005,xi:45–47.
-
Zhaoli Z, Hongyuan Fifty, Ye Y. Survey of factors associated with unprotected sexual behaviors among men who have sex with men in Beijing. Chin J Natural Med. 2008;10:241–5.
-
Yingjie LMYBW. Epidemiology characteristics, sexually transmitted affliction and HIV/AIDS condition among 403 female sex workers in Chaoyang Commune, Beijing. CHINESE JOURNAL OF DRUG DEPENDENCE. 2006;5:401–4.
-
Yan-jie G, MYSL. Prevalence and Predictors of HIV, syphilis and herpes simplex blazon 2 virus ( HSV-ii ) infections among the men who accept sex with men ( MSM ) in Beijing. Chin J Public Health. 2012;4:451–iii.
-
Dong-liang LIYGMY. Written report on the incidence of HIV and associated take a chance factors through a prospective cohort amidst men who take sex with men in Beijing, China. Chinese J Epidemiol. 2012;7:663–6.
-
Wei WYLSJ. Achievement of HIV AIDS program in the past years and challenges in China. Chinese J Epidemiol. 2015;12
-
Donnell D, Baeten JM, Kiarie J, Thomas KK, Stevens W, Cohen CR, et al. Heterosexual HIV-one manual after initiation of antiretroviral therapy: a prospective cohort analysis. Lancet. 2010;375:2092–eight.
-
Cohen MS, Chen YQ, McCauley M, Hazard T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early on antiretroviral therapy. Northward Engl J Med. 2011;365:493–505.
-
THE THAI WORKING GROUP ON HIV AIDS PROJECTIONS. The Asian epidemic model (AEM) Projections for HIV/AIDS in Thailand: 2005-2025[R].2005. In.
-
Jin F, Jansson J, Law M, Prestage GP, Zablotska I, Imrie JC, et al. Per-contact probability of HIV manual in homosexual men in Sydney in the era of HAART. AIDS. 2010;24:907–13.
-
Baggaley RF, White RG, Boily MC. HIV transmission risk through anal intercourse: systematic review, meta-analysis and implications for HIV prevention. Int J Epidemiol. 2010;39:1048–63.
-
Dongliang LI, Yanjie G, Mingrun Y, Xueying Y, Shuming L, Jie 10, Yingjie L. Study on the incidence of HIV and associated risk factors through a prospective accomplice among men who have sexual practice with men in Beijing, China. Chinese J Epidemiol. 2012;33:663–vi.
-
Beijing Chaoyang Commune Health bureau. twelfth Five-Year Planning of AIDS prevention and control in Chaoyang District, Beijing. In; 2012.
-
AA L, Northward H MS. Condom distribution in jail to preclude HIV infection. AIDS Behav. 2013;(eight):2695–702.
-
Montaner JS, Lima VD, Barrios R, Yip B, Wood E, Kerr T, et al. Association of highly active antiretroviral therapy coverage, population viral load, and yearly new HIV diagnoses in British Columbia, Canada: a population-based study. Lancet. 2010;376:532–nine.
-
Shafer LA, Nsubuga RN, Chapman R, O'Brien Grand, Mayanja BN, White RG. The dual bear on of antiretroviral therapy and sexual behaviour changes on HIV epidemiologic trends in Republic of uganda: a modelling study. Sex Transm Infect. 2014;90:423–9.
-
Ramadanovic B, Vasarhelyi K, Nadaf A, Wittenberg RW, Montaner JS, Wood E, Rutherford AR. Changing take a chance behaviours and the HIV epidemic: a mathematical assay in the context of treatment as prevention. PLoS 1. 2013;viii:e62321.
Acknowledgements
We thank Jiang Shulin, Wang Lijuan, Wu Wei, Yuan Shengnan, Zhu Junling, Song Liang, Yang Ye, Liu Jun, Hu Yao, and Meng Haiying in the Beijing Chaoyang District Middle for Affliction Control and Prevention for their inquiry assistance, and Lu Hongyan and Li Guiying in the Beijing Center for Disease Control and Prevention for their advice. We would similar to limited our thanks to Ma Ning at COFCO Corporation for his comments.
Funding
This study was supported by the National Primal Applied science Program from the 12th 5-Year Plan of Cathay (named "the written report of projection on the HIV epidemic and mathematical model prediction in China", 2012ZX10001001–002). The funding body had no role in the design of the study, the collection, analysis, and interpretation of data or in writing the manuscript.
Availability of data and materials
The datasets used and/or analysed during the electric current study are available from the respective writer on reasonable request.
Ideals blessing and consent to participate
Ethical approval and participant consent were not necessary, as this study involved the use of a previously published de-identified database according to [Upstanding review of biomedical research involving human beings], which was promulgated by National Health and Family Planning Commission of Cathay (http://world wide web.moh.gov.cn/fzs/s3576/201610/84b33b81d8e747eaaf048f68b174f829.shtml).
Writer information
Affiliations
Contributions
TLL conceived and designed the work that led to the submission and drafted the manuscript. LM revised the manuscript and contributed to model refinement. LSM contributed to data collection. LJ helped perform the assay. WN approved the terminal version. All authors have read and canonical the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Not applicative.
Competing interests
The authors declare that they take no competing interests.
Publisher'south Annotation
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/past/four.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Eatables license, and indicate if changes were made. The Creative Eatables Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Reprints and Permissions
Nigh this article
Cite this commodity
Tao, L., Liu, 1000., Li, S. et al. Condom use in combination with ART can reduce HIV incidence and mortality of PLWHA among MSM: a report from Beijing, People's republic of china. BMC Infect Dis eighteen, 124 (2018). https://doi.org/10.1186/s12879-018-3026-8
-
Received:
-
Accustomed:
-
Published:
-
DOI : https://doi.org/10.1186/s12879-018-3026-8
Keywords
- Condom use
- Antiretroviral therapy (ART)
- Man immunodeficiency virus (HIV)
Source: https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-018-3026-8
0 Response to "Community Intervention Hiv Msm 2015 Art With Condom Use"
Post a Comment